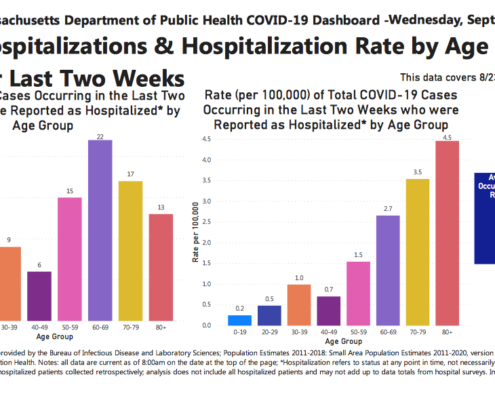
How did COVID impact Massachusetts’ long-term care facilities?
In April 2021, the Department of Public Health (DPH) removed from the COVID-19 Response Reporting Dashboard its former count of long-term care deaths, which was then greater than 9,000 – more than half of all reported COVID deaths at that time. In place of the count of long-term care deaths was a vague reference to various separate reports, one of which contained a total number of eldercare deaths that was thousands lower than the previously displayed number.
Pioneer reported this abrupt and substantial change in its May 2021 white paper, “A Brighter Dashboard: State Should Cut Confusion and Clarify Eldercare Cases and Deaths.” The paper asked, understandably, for a clear explanation: What counting methodology produced the 9,000-plus figure? And, if thousands of those deaths are no longer considered long-term care deaths, what are representative examples of such deaths? Addressing this question would help the public understand what was removed from the former total.
Pioneer pressed the Executive Office of Health and Human Services and DPH for such an explanation orally in virtual meetings and in writing through 2021, and was unsuccessful in those efforts. Subsequently, Pioneer has filed this Public Records Act request. How COVID impacted Massachusetts’ long-term care facilities is a matter of obvious importance, both on principle (the public has a right to know the facts), and for purposes of evaluating – and where possible improving – public policy. The state’s amendment of its long-term care death count may have been appropriate – but the public has the right to evaluate that question, and cannot do so absent a better explanation of what happened and why.
Get Our COVID-19 News, Tips & Resources!
Related Content: