Study: Growth of Antibiotic-Resistant Infections Could Have Massive Human, Financial Costs
Dysfunctional market, perverse incentives caused by Medicare reimbursement rates contribute to problem
BOSTON – The world was blindsided by COVID-19, but a new Pioneer Institute study finds that even as we continue to wrestle with the pandemic, another threat looms that scientists have long known about but the nation has thus far failed to address: the growth of antibiotic-resistant infections.
“Market dysfunction and perverse Medicare reimbursement rates have led to a growth in infections that resist antibiotics,” said Gunnar Esiason, author of “Antimicrobial Resistance: Learning from the current global health crisis to prevent another one.” If we don’t solve this problem, the human and economic costs are likely to be astronomical.”
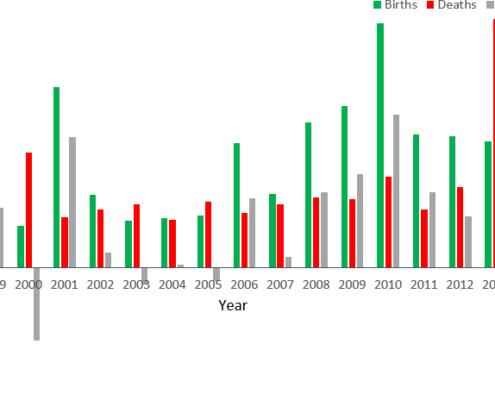
In the U.S., around two million people per year contract infections that are resistant to antibiotics and as many as 23,000 of them die. These drug-resistant infections account for $20 billion in health care costs.
If unchecked, it’s forecast that the problem could claim 10 million lives per year worldwide and be responsible for the loss of $100 trillion in economic output by 2050.
Antibiotic resistance is driven by years of overuse and misuse of antibiotics. Medicare is the nation’s largest payer, and its recipients account for the majority of resistant infections. Because hospitals receive the same reimbursement whether they use an older generic drug or a new drug that is likely to be more expensive, there is a financial incentive to prescribe the older drugs, even if those drugs may not be as effective because patients have built up resistance to them.
The continuing use of older drugs exacerbates the antibiotic resistance problem. It can also result in higher health care costs because additional treatments are required to treat the infection, or cause hospitals to use unnecessarily strong antibiotics to treat it effectively.
Hospitals favoring older generic drugs even if they are less effective makes it harder for new drugs to recoup development costs, which can be up to $2.6 billion. As a result, investment is down and the number of new antibiotics approved by the FDA has fallen in recent years. In addition, companies working on new antibiotics are more likely to be small firms or start-ups that are less financially stable.
With its large concentration of life science companies, Massachusetts could be particularly hard hit if investment in new antibiotics continues to lag.
One effort to address the antibiotic-resistant infection problem is the DISARM Act, which was introduced in Congress last year. The legislation would increase Medicare antibiotic reimbursements and eliminate the incentive to prescribe less expensive drugs that are often less effective by allowing for the reimbursement of all antibiotics, regardless of cost. Backers argue that the bill would slow the growth of resistant infections by ending the overuse of older drugs that have become less effective, and that newer, more effective antibiotics could reduce long-term costs.
Esiason also recommends mounting a broad awareness campaign that would tie this impending public health and economic threat to our current battle against COVID-19.
About the Author
Gunnar Esiason is a cystic fibrosis and rare disease patient leader, who is passionate about early stage drug development, patient empowerment and health policy. He is a second-year M.B.A. student at the Tuck School of Business at Dartmouth and is also working towards a Master of Public Health degree at the Dartmouth Institute for Health Policy and Clinical Practice. At Tuck, Gunnar serves as a Tuck Center for Health Care MBA Fellow, a health care club co-chair and a club hockey captain. Prior to Tuck, Gunnar received a BA form Boston College in 2013, worked on an enteral feeding product at a medical nutrition company, was appointed to the board of directors at the Boomer Esiason Foundation, and was the head coach of his high school alma mater’s varsity hockey team. Gunnar maintains the roles of patient advocate and director of patient outreach at the Boomer Esiason Foundation.
He has consulted on clinical trial development, a real-world evidence population health study, and a cystic fibrosis-specific mental health and wellness screening tool. In 2019, Gunnar delivered the pre-commencement address at the St. Louis University School of Medicine commencement exercises. He has also been featured as a keynote speaker at more than two-dozen top medical centers, biotech conferences, and health industry events across the United States. His health policy opinions have been featured in Newsweek, The New York Daily News, The Hill, US News & World Report, and Morning Consult.
About Pioneer
Mission: Pioneer Institute develops and communicates dynamic ideas that advance prosperity and a vibrant civic life in Massachusetts and beyond.
Vision: Success for Pioneer is when the citizens of our state and nation prosper and our society thrives because we enjoy world-class options in education, healthcare, transportation and economic opportunity, and when our government is limited, accountable and transparent.
Values: Pioneer believes that America is at its best when our citizenry is well-educated, committed to liberty, personal responsibility, and free enterprise, and both willing and able to test their beliefs based on facts and the free exchange of ideas.
Get Updates On Our Life Sciences Work!
Related Posts