New Report Addresses Distinct Challenges in Utilizing ICER to Assess Value of Rare Disease Treatments
Pioneer Institute Discourages Policymakers & Payers from Adopting ICER to Evaluate Rare Disease Treatments
Media inquiries: Contact Micaela Dawson, 617-723-2277 ext. 203 or mdawson@pioneerinstitute.org
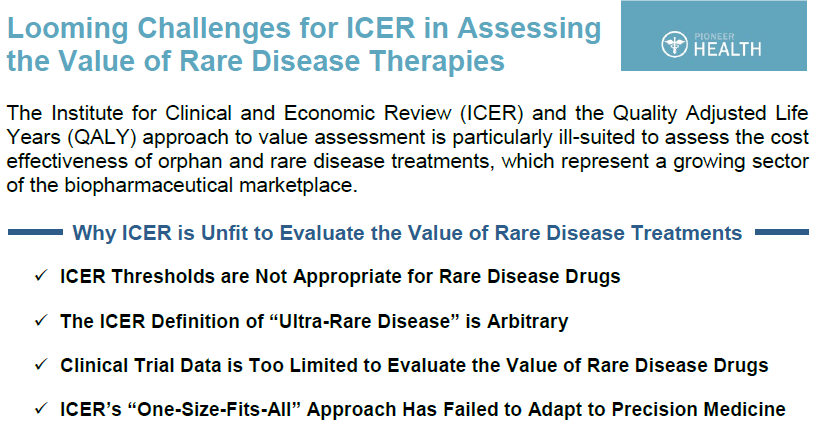
BOSTON, MA – Today, Pioneer Institute released a new report, Looming Challenges for ICER in Assessing the Value of Rare Disease Therapies, that examines why the Institute for Clinical and Economic Review (ICER) and the Quality Adjusted Life Years (QALY) approach to value assessment is particularly ill-suited to assess the cost-effectiveness of orphan and rare disease treatments, which represent a rapidly growing sector of the biopharmaceutical marketplace. In the report, lead author and Pioneer Institute Visiting Fellow in Life Sciences, Dr. William Smith illustrates a number of reasons why ICER is unfit to evaluate the cost-effectiveness of rare disease treatments, including:
- ICER thresholds are not appropriate for rare disease drugs;
- ICER’s definition of “ultra-rare disease” is arbitrary;
- Clinical trial data is too limited to evaluate the value of rare disease drugs; and
- ICER’s “one-size-fits-all” approach has failed to adapt to precision medicine.
With the recent growth in medicine spending, state and federal policymakers and payers are exploring the use of cost-effectiveness reviews to evaluate drugs for smaller patient populations with complex and rare diseases. Dr. Smith argues that ICER and QALY are not appropriate to meet that need.
“The ICER QALY thresholds are arbitrary enough when applied to traditional medicines but when applied to treatments for rare diseases, they take on additional – and troubling – arbitrariness…These thresholds are not “scientific” in any economic sense but, in asserting a value on human life, they are a kind of theological dogma that must be accepted on faith as an objective standard.”
As Dr. Smith points out, ICER itself has acknowledged the challenges that exist in evaluating the growing number of drugs for complex and rare diseases, and has unsuccessfully attempted to revise its value framework to meet the unique challenges associated with this segment of medicine. Between 2014 and 2018, none of ICER’s reviews of rare disease drugs resulted in a “high value” rating. A recent ICER review of two breakthrough treatments for Spinal Muscular Atrophy (SMA) concluded that neither therapy met “traditional cost-effectiveness thresholds.”
“Research and development costs for a rare disease drug are quite substantial as finding and enrolling patients in trials are particularly challenging. And with lower prevalence rates, these higher costs are spread over much smaller patient populations, making the prices for one course of treatment substantially higher than traditional small molecule drugs for large patient populations.”
The report also examines ICER’s unwillingness to appropriately adjust its methodology for orphan and rare diseases. In 2017, ICER created a new “ultra-rare” category of diseases with patient populations of less than 10,000, a classification which does not correspond to any accepted definition of rare or ultra-rare diseases. It drew scrutiny from the patient advocacy community, including the National Organization for Rare Disorders (NORD).
“Given the arbitrary nature of ICER’s definition of rare diseases as well as their QALY thresholds, they were likely chosen to cast the widest possible net for their broader and more severe price control regime that is at the heart of the ICER model.”
Pioneer Institute discourages policymakers and payers from adopting ICER and other “one-size-fits-all” cost-effectiveness models, especially for those innovative and groundbreaking therapies to treat orphan and rare diseases. Instead, Pioneer Institute believes patients, their physicians and caregivers, and a variety of other societal factors should determine the value of these therapies.
“ICER’s continuing negative reviews of rare disease drugs seem to indicate that their goal is not to accommodate the unique contextual challenges of rare disease therapies but simply to push their prices down.”
About the Author
William Smith is Visiting Fellow in Life Sciences at Pioneer Institute. He has 25 years of experience in government and in corporate roles, including as vice president of public affairs and policy at Pfizer, and as a consultant to major pharmaceutical, biotechnology and medical device companies. He held senior staff positions for the Republican House leadership on Capitol Hill, the White House, and in the Massachusetts Governor’s office.
About Pioneer
Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.
Click image below to download our handout on this report:
Get Updates On Our Healthcare Research and Events!
Make a tax-deductible gift below to support our work to protect patients.
Recent healthcare posts: