MA Health Insurers Have Made Good Progress in Price Transparency, But Significant Work Remains
Read press coverage of this report in the Boston Business Journal and State House News Service.
Tools are more user friendly and cover growing number of procedures, but still used by just a small fraction of potential market
BOSTON – A Pioneer Institute study finds some significant improvements in the online cost estimator tools created by Massachusetts’ three largest health insurers, but there is much still to be done for the carriers to maximize the opportunity price transparency represents.
Online cost estimator tools give consumers/plan members online information about a range of information for outpatient and many inpatient procedures. These tools display the amount that has to be paid by consumers to any particular provider, how much the plan pays the provider, and information about provider quality. Consumers can compare several providers at the same time.
“Price transparency can help initiate reforms that reduce healthcare costs and allow market forces to drive patients to lower-cost, higher-value providers,” said Barbara Anthony, primary author of MA Health Insurers Have Improved Their Consumer Price Transparency Efforts, But Significant Work Remains.
A 2012 state law required health insurers to develop online cost estimator tools by October 2014. In 2015, the advocacy group Health Care for All (HCFA) assessed the tools developed by Blue Cross Blue Shield (BCBS), Harvard Pilgrim Health Care (HPHC), and Tufts Health Plan, which together controlled nearly four-fifths of the state health insurance market. HCFA gave each a grade of “C.”
The same law also requires hospitals and doctors to provide consumers with prices of services upon request. Previous Pioneer studies showed very poor compliance by Massachusetts providers with the Commonwealth’s transparency law.
As a follow up to the HCFA study, in late 2017, Pioneer assessed the same carriers’ performance and found their tools more user friendly. They cover between 700 and 1600 procedures, a vast improvement over the initial numbers of procedures available in 2015. Importantly, Pioneer found that all three carriers are embracing incentive/reward programs to attract workers at entities with 250 or more employees to lower-cost, high-value providers. Pioneer’s study was done with the full cooperation of the carriers.
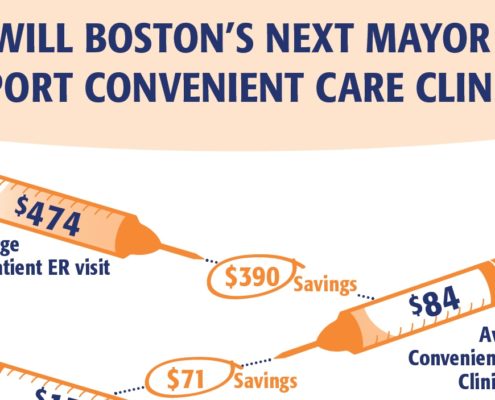
Under incentive/rewards programs, employees are rewarded by either small or no co-payments or cash rewards from $25 to several hundreds of dollars for choosing lower-cost, high-value providers such as outpatient surgical centers rather than a hospital outpatient clinic. HPHC has developed a program called SaveOn that makes it easier for members to switch providers to avoid co-pays or earn cash rewards. BCBS has aggressively embraced and marketed cash incentive programs to both businesses and municipalities. In all cases, the plans say they are embracing incentive programs and transparency to compete with large national carriers here and regionally.
Both the HPHC’s and THP’s tools are a significant improvement over their initial cost estimator tools. After their common vendor pulled out of the market, the carriers had to entirely revamp their tools. The results are new, easy-to-navigate online tools which display out-of-pocket consumer costs, the remaining deductible, and quality metrics.
Since 2015, BCBS has made several improvements that make its product more consumer friendly: by simply changing the name of its tool from “Find a Doc” to “Find a Doc and Estimate Costs,” by making the tool much more prominent on its website, and clearly showing both out-of-pocket costs and remaining deductibles. BCBS also has an improved website for consumers.
Despite significant progress, however, deficiencies remain. The carriers had about 297,000 aggregate inquiries on their cost estimator tools from early 2014 through 2017, compared to a potential market of at least three million people that the three carriers cover.
“The number of aggregate inquiries shows that carriers still have a lot of work ahead to achieve price transparency’s potential to rein in healthcare costs,” said Pioneer Institute Executive Director Jim Stergios.
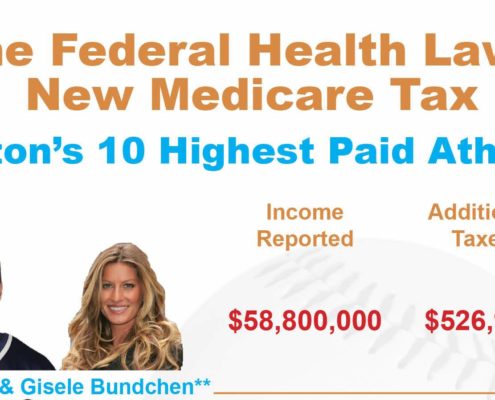
In 2015, Massachusetts’ median annual household income was around $70,000 and the average family in the Commonwealth spent about $20,000 on premiums and cost sharing. “These figures show that transparency in healthcare is important to the budgets of Massachusetts families,” added Stergios.
HPHC’s and Tufts’ estimator tools still don’t provide cost data on many behavioral health procedures.
The BCBS site is compatible with online translation tools, but none of the carriers’ cost estimator tools are readily available in a language other than English.
Anthony noted that “While state government has not provided any compliance leadership for consumer price transparency, now, after overcoming resistance and a lack of support, the market is waking up to the potential benefits of price transparency and incentive programs.”
Comments from Harvard Pilgrim Health Care, Blue Cross Blue Shield and Tufts Health Plan:
“In a rapidly changing healthcare environment, providing consumers with transparency around cost and quality information is important and will help them make informed healthcare choices,” said Harvard Pilgrim President and CEO Eric Schultz. “We at Harvard Pilgrim have long been committed to promoting the value of transparency, and we are pleased to see that Pioneer Institute continues to keep a public focus on the issue. We were happy to work with them on this report.”
“Blue Cross is pleased that the Pioneer report acknowledges our ongoing commitment to providing our members with state-of-the-art tools to make informed decisions about the cost and quality of their healthcare. Members who understand their benefits – those who aren’t surprised by bills and feel empowered – are much more likely to be satisfied members and engaged patients. I thank Pioneer Institute for their continued focus on this issue,” said Andrew Dreyfus, BCBS President and CEO.
“Transparency is essential among all stakeholders in healthcare to ensure that customers and employer groups can make informed healthcare decisions,” said Tom Croswell, President and CEO at Tufts Health Plan. “[O]ur new, easy-to-use tool enables members to not only find high-quality, high-value providers in their area, but also see their potential costs from the beginning to the end of a procedure. The new tool is simpler and far surpasses the capabilities of the first generation of transparency tools. We applaud Pioneer Institute’s work on keeping this important issue at the forefront.”
About the Authors
Barbara Anthony, a lawyer, is a senior fellow in healthcare at Pioneer Institute focusing on healthcare price and quality transparency. She is also an associate at the Harvard Kennedy School’s Center for Business and Government. She served as Massachusetts Undersecretary for Consumer Affairs and Business Regulation from 2009 to 2015.
Scott Haller graduated from Northeastern University with a Bachelor’s Degree in Political Science. He started working at Pioneer Institute through the Northeastern’s Co-op Program and continues now as the Lovett C. Peters Fellow in Healthcare. He previously worked at the Office of the Inspector General.
About Pioneer
Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.
Get Updates On Our Healthcare Research and Events!
Related Posts