Moving the Needle on Healthcare Cost Containment & Reform
/0 Comments/in Blog, Blog: Healthcare, Blog: Healthcare Transparency, Blog: Medicaid, Featured, Healthcare /by Editorial StaffToday, Pioneer Institute submitted recommendations to the Commonwealth of Massachusetts’ Special Senate Committee on Health Care Cost Containment and Reform. Pioneer applauds provisions of the proposed legislation that would reduce emergency room use and re-admissions, expand scope of practice, and embrace telemedicine. The Committee should also be commended for looking to other states’ accomplishments in this area.
But the current bill raises some concerns. In some instances, we believe it diminishes the potential for greater cost savings by adding unnecessary regulatory burdens. The projected savings relative to 2020 spending are quite modest, at less than 0.2 percent. The Medicaid buy-in program as it is presented is a radical change from the existing program structure – it will require more elaboration and analysis, as it is unclear what the impact of this proposal will be on MassHealth and providers across the Commonwealth. Pioneer also has concerns that the bill could lead to harmful unintended consequences, such as the collapse of the merged private insurance market. We hope the Legislature addresses these issues, but this bill starts an important healthcare cost conversation in Massachusetts, and we commend the Senate for taking the lead in this effort. Read Pioneer’s full letter to the Committee.
Get Updates On Our Healthcare Research and Events!
Related Research

An Evaluation of 340B in Massachusetts

Do No Harm to the Health Policy Commission
New Online Tool Tracks MA Hospital Revenue from Commercial Sources
Middlemen Pushing Up Retail Costs of Drugs

Telehealth Progress Slowed in 2023

‘High’ U.S. Drug Prices Mask Freeloading by Other Nations

University Science Research Is Under Threat
Opinion: Legislature should act on bill to limit out-of-pocket drug costs

Healthcare: Suffolk County’s Biggest Driver for Labor and Employment

Opinion: Drug patents aren’t a ‘necessary evil.’ They save lives.

Study: High List Prices and Deep Discounts for Prescription Drugs Hurt Poor and Sick Patients

Massachusetts’ Misguided Middle-Class Health Insurance Subsidy Expansion

Study: Massachusetts Should Join 45 States and Allow Prescribers to Dispense Medications

A Federal Drug Discount Program for the Wealthy

Sunshine Week 2023: Shining Light on the Workings of Government

As COVID-19 Emergencies Ease, Some Progress on Telehealth Rules
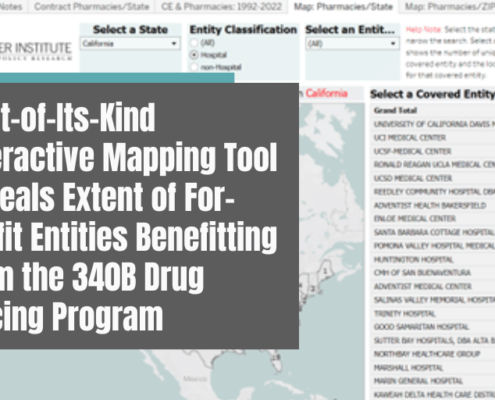
First-of-Its-Kind Interactive Mapping Tool Reveals Extent of For-Profit Entities Benefitting from the 340B Drug Pricing Program