National Study Finds Most States Lack Healthcare Price Transparency Laws
33 states either have weak or no price transparency laws at all
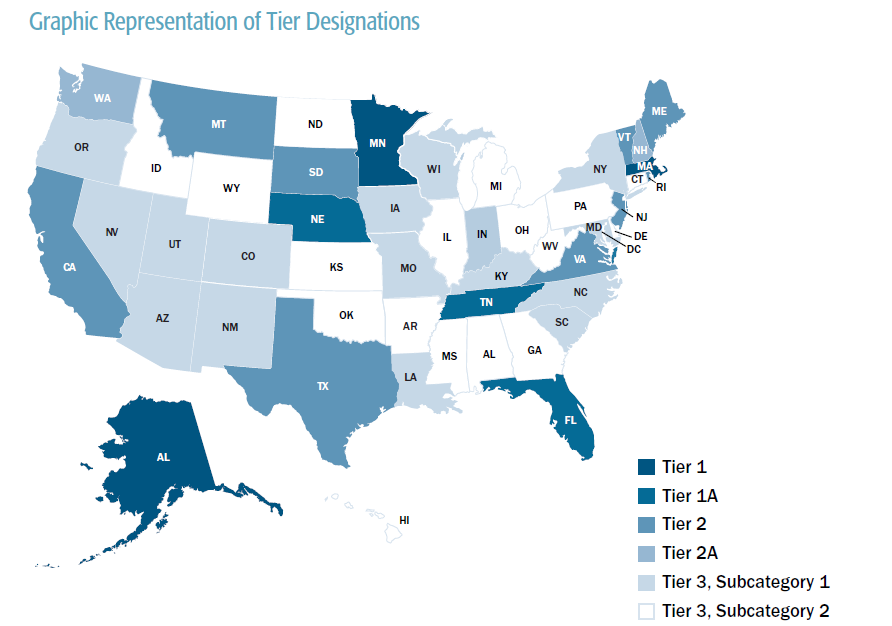
BOSTON – At a time when the coronavirus pandemic has caused massive shifts in state policies on telehealth and scope of practice in healthcare, a new Pioneer Institute study underscores that most of the 50 states continue to suffer from weak laws regarding price transparency. The study identified states that have laws that require carriers, providers or both to provide personalized cost information to consumers before obtaining healthcare services. Fully 33 states placed in the lowest of the three broad analytic tiers on the strength of their state healthcare transparency laws.
“Robust price transparency laws are clearly not widespread in the U.S.,” said Barbara Anthony, a co-author of “Status of Healthcare Price Transparency Across the United States.”
Alaska, Massachusetts, and Minnesota placed in the highest tier, which requires both providers and insurance carriers to supply price information that reflects, to the greatest degree possible, the amount a consumer would have to pay for a medical procedure.
“This study provides a snapshot of the statutory requirements in our 50 states. That’s the baseline where the conversation on patient access to prices must start,” said Jim Stergios, executive director of Pioneer Institute. “While Massachusetts and five other states have, according to our analyses, the strongest legal requirements in the country, the competition is not steep. We have a long way to go.”
Under Massachusetts law, both providers and carriers are required to make price estimates available within two business days of a request received via email or phone.
Carriers are required to provide a website and toll-free number that allow consumers to obtain real-time estimates and facilitate comparisons among care options. The carriers must not only show a consumer’s out-of-pocket costs, but also the amount remaining on his or her deductible.
Rounding out the six states with the strongest laws are Florida, Nebraska, and Tennessee, which require either providers or carriers to supply price information.
The remaining states fall into Tiers 2, 2A and 3:
- The study categorizes laws in nine states as Tier 2, which means they require price estimates when certain conditions are met.
- New Hampshire and Washington are categorized as Tier 2A, which means they offer web tools that provide comprehensive price estimates even though the tools are not required by law.
- About two thirds of the states – 33 in all – fall into Tier 3, meaning they have no laws regarding personalized price estimates, although about half of these states offer some type of web tool that provides some more general, non-personalized, cost information.
The authors offer states three main recommendations to improve healthcare price transparency. First, states should require or create incentives for making personalized cost estimates available in all non-emergent cases.
A recent Massachusetts survey of insured workers found that while 70 percent wanted to know the out-of-pocket cost for any medical procedure before it was performed, most do not know how to access such information even though it is available. Given this under-utilization of so-called cost estimator tools, the authors recommend that states partner with employers, carriers, and providers to create methods to educate individuals about the tools and resources available to them.
According to Anthony, “It’s no surprise that patients want to know how much treatments will cost, given that health insurance policy deductibles can be more than $7,000.”
Finally, Pioneer calls for leveraging the value of cost estimator tools by requiring that the tools make it easy for consumers to not only access cost information, but to make it easy to compare prices among various providers. In addition, the report recommends that carriers and employers focus more on providing cash rewards to incent consumers to choose high value/lower cost providers.
“With the pandemic upending many long-term arrangements among the various industry players, now is the time to give patients the same kind of information they have in every other part of their lives,” said Jim Stergios. “The polling shows that, while Massachusetts fares better on its statutes, the implementation of the law shows that patients want action and less talk.”
The study also describes recent efforts by the federal government to require more hospital and carrier price transparency. Readers will find the report heavily annotated and rich with references to state laws across the country as well as to numerous websites operated by various states.
About the Authors
Caterina DiBiase, the primary author of this report, is graduating this Spring with a Masters Degree in Public Policy from the University of Massachusetts in Amherst where she specialized in social justice and public health. She was a member of the accelerated masters degree cohort. From September 2019 to January 2020, Caterina served as a Pioneer Research Assistant in Healthcare Policy working with Senior Fellows on various healthcare projects including healthcare price transparency and direct primary care in Massachusetts.
Lauren Corvese is Pioneer’s Annual Fund Director. She joined Pioneer in 2015 as a co-op student, writing on education, healthcare, and transportation policy in Massachusetts. Lauren recently earned a Bachelor of Arts in Political Science from Northeastern University, where she graduated summa cum laude.
Scott Haller graduated from Northeastern University with a Bachelor’s Degree in Political Science. He started working at Pioneer Institute through Northeastern’s co-op program and was the Lovett C. Peters Fellow in Healthcare. He previously worked at the Massachusetts Office of the Inspector General.
Barbara Anthony, lawyer, economist, and public policy expert, is a Senior Fellow in Healthcare Policy at Pioneer Institute. She was also a former Senior Fellow and Associate at the Harvard Kennedy School’s Center for Business and Government where she researched and wrote about Massachusetts market reform and healthcare cost containment efforts. She served as Massachusetts Undersecretary of the Office of Consumer Affairs and Business Regulation from 2009 to 2015 and has worked at the intersection of federal and state commercial regulation and the business community for many years. Anthony’s work has appeared in numerous state and national publications.
Josh Archambault is a Senior Fellow at Pioneer Institute. Prior to joining Pioneer, Josh was selected as a Health Policy Fellow at the Heritage Foundation in Washington, D.C. In the past, Josh served as a Legislative Director in the Massachusetts State Senate and as Senior Legislative Aide in the Governor’s Office of Legislative Affairs. His work has appeared or been cited in numerous news outlets. He is the editor and coauthor of The Great Experiment: The States, The Feds, and Your Healthcare. Josh holds a Master’s in Public Policy from Harvard University’s Kennedy School and a BA in Political Studies and Economics from Gordon College.
Seher Chowdhury is graduating this Spring from the Boston University School of Public Health (BUSPH) with a Masters Degree in Public Health; her areas of specialization include Health Policy & law and Epidemiology and Biostatistics. She has been a Pioneer Research Assistant in Healthcare Policy since June 2019. She has worked extensively in the area of healthcare price transparency along with Pioneer’s Senior Fellows.
Mission: Pioneer Institute develops and communicates dynamic ideas that advance prosperity and a vibrant civic life in Massachusetts and beyond.
Vision: Success for Pioneer is when the citizens of our state and nation prosper and our society thrives because we enjoy world-class options in education, healthcare, transportation and economic opportunity, and when our government is limited, accountable and transparent.
Values: Pioneer believes that America is at its best when our citizenry is well-educated, committed to liberty, personal responsibility, and free enterprise, and both willing and able to test their beliefs based on facts and the free exchange of ideas.
Get Updates On Our Healthcare Cost Transparency Initiative!
Related Content