Follow-Up Survey Finds Hospitals Still Fall Short On Price Transparency
Estimated price of routine procedure at 21 Massachusetts hospitals shows price variations of up to 1,000 percent
Read media coverage of this report in The Boston Globe, the Boston Herald, the Springfield Republican, Beckers Healthcare, State House News Service. Healthcare Finance, and The Lowell Sun.
BOSTON – Eighteen months after an initial survey found little price transparency at Massachusetts hospitals, a follow-up study from Pioneer Institute reveals that it remains highly unlikely that ordinary consumers can get a hospital price estimate within two business days of requesting it, as required by state law.
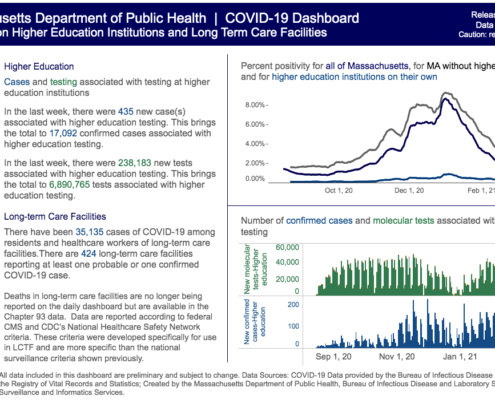
For “Massachusetts Hospitals Score Poorly on Price Transparency… Again,” researchers called 21 hospitals that had been part of the earlier survey to again request a self-pay estimate for an MRI of the left knee without contrast. Only nine of the hospitals were able to provide the estimate within two business days.
“Deductibles can range from $1,500 to more than $7,000,” said Pioneer Senior Fellow in Healthcare Policy Barbara Anthony, who authored the report with Scott Haller. “Given that reality, access to price information is more important than ever before. This survey once again demonstrates how frustrating and time consuming it is for the average consumer to obtain a price quote. ”
Unlike in the first survey, callers also asked about self-pay or cash discounts, which ranged from 6-to-47 percent.
There was wide variation in the prices quoted. Undiscounted estimates ranged from $1,061.22 at Morton Hospital and Medical Center in Taunton to $8,447 at Boston’s Massachusetts General Hospital. Discounted estimates, which is the price for a self-pay patient, went from $636.73 at Morton to $6,928 at MGH.
About two thirds of the hospitals readily disclosed the self-pay discount, while in the other cases callers had to ask about it. MRI reading fee discounts were disclosed at a similar rate.
While state law requires that price estimates be given within two business days, it took an average of two-to-four business days to get pricing information. Response time ranged from a few minutes at Baystate Franklin Medical Center in Greenfield and Morton Hospital and Medical Center in Taunton, to six or seven days at some other hospitals.
Five of the 21 hospitals required callers to supply a diagnostic code before providing an estimate, which may violate state law. Several others asked for one, but hospital personnel eventually looked up the code – which is much more accessible to the institutions than it is to patients.
Some hospitals directed callers to a third party to get a separate estimate for the MRI reading fee, which can delay receipt of a quote by 48 hours or more. However, Lahey Hospital and Medical Center and Newton-Wellesley Hospital provided a consumer-friendly global price.
To check the reliability of price estimates, researchers called hospitals back at least a month after getting their original estimate. Seven hospitals provided different prices the second time. Six ranged from 2.7 percent above the original estimate at South Shore Hospital to 76.7 percent higher at MGH. Most of these different estimates resulted from mistakes made by hospitals during the first call. The second estimate from MetroWest Medical Center was 22 percent lower.
“I think there are two major takeaways from these surveys,” said Pioneer Executive Director Jim Stergios. “The first is that three years after it took effect, the time has come for hospitals to get serious about complying with the state’s price transparency law, and the second is that state government needs to exercise leadership and do a much better job of advancing compliance with these laws.”
About the Authors
Barbara Anthony, a lawyer, is a senior fellow in healthcare at Pioneer Institute focusing on healthcare price and quality transparency. She is also an associate at the Harvard Kennedy School’s Center for Business and Government. She served as Massachusetts Undersecretary for Consumer Affairs and Business Regulation from 2009 to 2015.
Scott Haller graduated from Northeastern University with a Bachelor’s Degree in Political Science. He started working at Pioneer Institute through the Northeastern’s Co-op Program and continues now as the Lovett C. Peters Fellow in Healthcare. He previously worked at the Office of the Inspector General.
Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.
Get Updates On Our Healthcare Cost Transparency Initiative!
Join us on May 3rd, for our annual Hewitt Healthcare Lecture, “Evolving Healthcare Delivery Models”:
Paul F. Levy, former President & CEO, Beth Israel Deaconess Medical Center, will moderate a panel discussion on the changing face of the healthcare market and innovations to meet consumer demand. Learn more!


 This file is licensed under the Creative Commons Attribution 2.0 Generic license.
This file is licensed under the Creative Commons Attribution 2.0 Generic license.