Survey Shows Wide Variation in Both Overall Cost of Medical Procedure and Amount Paid by Consumers
Making all-payer claims data public could put downward pressure on high-cost providers, reduce overall healthcare costs
BOSTON – Data from the Massachusetts Center for Health Information and Analysis (CHIA) show wide variations in the prices agreed to between individual insurers and providers, the portion paid by insurers and the amount that is consumers’ responsibility to pay, according to a new policy brief published by Pioneer Institute.
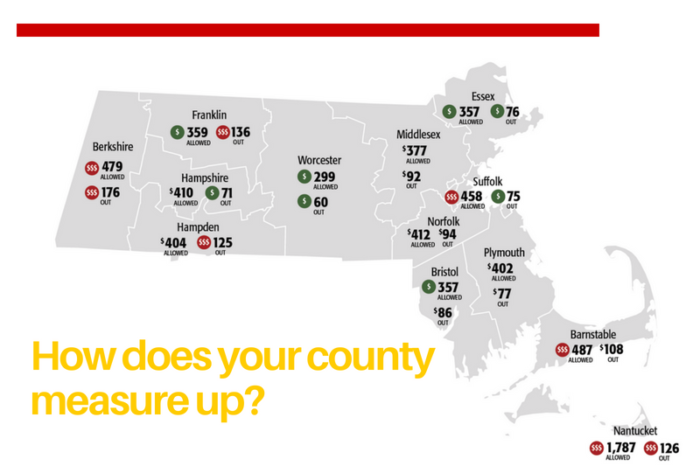
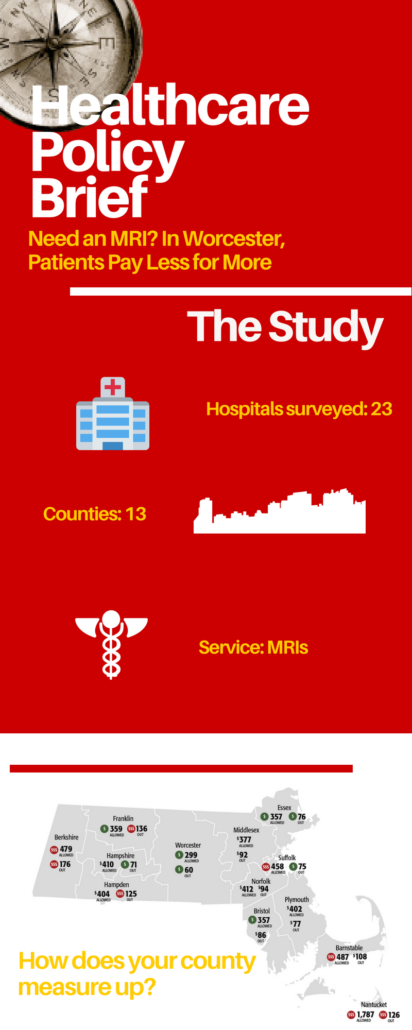
In “Need an MRI? In Worcester, Patients Pay Less for More,” author Scott Haller looks, by county, at various costs associated with a simple MRI of the knee. The data in the brief come from CHIA’s all-payer claims database (APCD), which warehouses medical claims data across the Commonwealth.
“Through CHIA, the state collects data that provide a window into the true cost of healthcare among various providers,” said Pioneer Executive Director Jim Stergios. “In an era of high-deductible plans, the state must make this information easily available to businesses and consumers. Without it, they cannot make smart choices about their medical care.”
Average “allowed amounts,” the price for a particular procedure agreed to between specific insurers and providers, ranged from $299 in Worcester County to $1,787 in Nantucket. The average amount paid by insurers went from a low of $213 in Worcester to $1,571 in Nantucket, and average consumer out-of-pocket costs varied from $60 in Worcester County to $176 in Berkshire County.
There were large price variations both between and among counties. Maximum out-of-pocket costs were $744 in Essex and Plymouth Counties, compared to $4,479 in Barnstable.
Data showing comparatively higher out-of-pocket costs in rural counties like Berkshire, Franklin, Nantucket and Hampden, which had the highest average out-of-pocket costs, suggest that high-deductible insurance plans are more common in those areas.
While Suffolk County had the fourth highest average allowed amount, its out-of-pocket average was third lowest among the 13 counties included in the brief (there is no MRI machine in Dukes County, more commonly known as Martha’s Vineyard), which suggests the prevalence of more generous insurance plans.
With both the lowest allowed amount (about $299) and out-of-pocket costs (around $60), patients in Worcester County appear to be getting the best overall deal in Massachusetts.
The brief also calls for making the APCD public. “Anyone with a deductible or co-insurance could save money if prices were readily available for comparison,” Haller said. “If enough consumers start shopping for their healthcare, it would put downward pressure on high-priced providers, leading to lower premiums and overall healthcare costs.”
About the Author
Scott Haller graduated from Northeastern University with a Bachelor’s Degree in Political Science. He joined Pioneer Institute through Northeastern’s Co-op Program and continues now as the Lovett C. Peters Fellow in Healthcare. He previously worked at the Massachusetts Office of the Inspector General.
About Pioneer
Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.
Get Updates On Our Healthcare Cost Transparency Initiative!
Related Research:








 This file is licensed under the Creative Commons Attribution 2.0 Generic license.
This file is licensed under the Creative Commons Attribution 2.0 Generic license.