Consumer Driven Health Care a Proven Cost-Saving Strategy
Massachusetts lags behind other states in adopting plans that use consumer engagement to reduce costs and improve the quality of care
BOSTON – As part of a push to contain health care cost growth, business leaders, state administrators, and policymakers should focus on Consumer Driven Health Care (CDHC) plans that involve consumers in making health care decisions, according to a Pioneer Institute report issued today.
Consumer Driven Health Care: A New Agenda for Cost Control in Massachusetts
The author of Consumer Driven Health Care: A New Agenda for Cost Control in Massachusetts is Dr. Amy Lischko, a senior fellow at Pioneer Institute and an associate professor at Tufts University School of Medicine. Lischko’s past experience includes serving as Commissioner of the Division of Health Care Finance and Policy, and numerous consulting engagements with AcademyHealth, Mathematica Policy Research, the National Governor’s Association, and individual states.
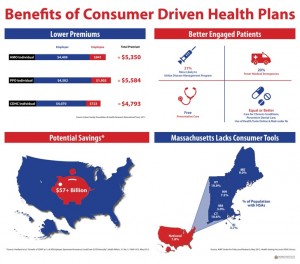
View Infographic.
Massachusetts faces two critical health care challenges. Health care costs borne by Massachusetts’ employers and employees are among the nation’s highest, and the commonwealth’s high insurance premiums disproportionately impact low-income working families.
In an effort to control costs earlier this year, the Massachusetts Legislature passed Chapter 224, a law that granted preference to alternative payment contracts and Accountable Care Organizations. This “supply-side” approach leaves health care decisions largely outside consumers’ control.
“The new state health care law, formally known as Chapter 224, will not succeed unless consumers are engaged,” said Pioneer’s Director of Health Care Policy Josh Archambault. “Patients need to be value-seekers for routine care, rewarding medical professionals who provide lower cost, high-quality care. Otherwise, the government will be in the business of containing costs through informal – or perhaps formal – rationing of care.”
In Consumer Driven Health Care, author Amy Lischko recommends coupling this law with a “demand-side” approach to cost containment, such as Consumer Driven Health Care (CDHC) plans. These plans have been shown to reduce health care spending, engage consumers and improve health more than traditional plans
Drawing on a review of recent literature and interviews with brokers, employer groups, and insurers, Dr. Lischko provides a historical perspective on CDHC in Massachusetts, exploring how it can help constrain heath care costs and increase patient engagement in health care decision-making.
“I was surprised by the availability of information regarding costs and quality, and by how well these plans have adapted to trends in the marketplace to address consumers’ concerns about preventive care,” remarked Dr. Lischko.
Critics mistakenly consider CDHC plans to be simply a high-deductible health plan, or a vehicle for employers to shift costs. But the report finds that recent changes in plan design have addressed most concerns raised. Evidence from both the private market and public programs shows that adopting CDHC plans has translated into tens of millions in savings for patients, employers, and government.
For patients, CDHCs can result in as much as 28 percent lower premium contributions, savings through a tax-advantaged health account that covers more out-of-pocket expenses, and increased engagement in preventive health programs.
For employers, CDHCs can result in premium contributions that are as much as 20 percent lower in the first year, average savings of $1,500 per employee, and healthier employees.
For state governments, the most promising of these programs’ is Indiana’s, which began offering its CDHC plans with health savings accounts in 2006, and has enrolled 90 percent of the state workforce. Enrollees saved $7-8 million in 2010.
In Massachusetts, significant government regulatory involvement in the insurance marketplace, along with a culture of generous coverage and the prevalence of HMOs, has left the state far behind others in embracing CDHC.
Dr. Lischko recommends concrete actions that state and federal policymakers and employers can take to improve access to these plans, including:
o State policymakers must revisit the empirical data on outcomes of CDHC plans
o State policymakers must ensure that the public has access to data on the cost of health care services
o The Group Insurance Commission should be required to offer CDHC plans with HSAs as an option for the state workforce
o Employers should offer CDHC plans with HSAs alongside traditional plans, educate and engage their workforce regarding health care decision-making, and add wellness benefits
“Managed care and capitation without consumer engagement was a dismal failure because consumers did not understand it, and fought against the very mechanisms that kept their premiums constrained,” said Dr. Lischko. “CDHC plans can complement Massachusetts’ approach to lowering costs.”
This is the first in a series of reports by Pioneer’s Center for Health Care Solutions aimed at improving patient-centered approaches to limiting health care costs in Massachusetts. Recent research has included: Impact of the Federal Health Law’s “Cadillac Tax” in Massachusetts, Business Solutions to the Health Care Cost Crunch, and Pioneer’s critically acclaimed book on state-driven health care reform, The Great Experiment. [Learn more at: http://greatexperiment.org/]
###
Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.