
Do No Harm to the Health Policy Commission
With only weeks left in the Massachusetts legislative calendar,…
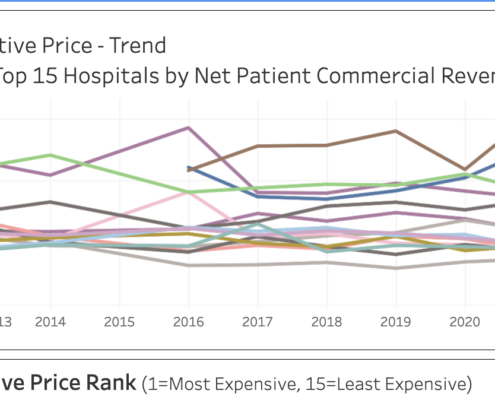
Boston Children’s, MGH Among Massachusetts Hospitals with Highest Relative Commercial Prices
Pioneer Institute's new tool, the Massachusetts Hospital Relative Price Tracker, displays relative price and facilitates relative price comparisons among hospitals. The average price among all hospitals will have a relative price of 1.0. A relative price of 1.5 means that a hospital charges 50 percent higher than the average of all Massachusetts hospitals. Similarly, a relative price of 0.84 means that a hospital’s prices are 16 percent below average. Relative price data is collected and reported by the Commonwealth’s Center for Health Information and Analysis (CHIA) and is an aggregate measure used to evaluate price variations among different hospitals. It is recalculated annually based on data collected from commercial payers and includes information on private commercial insurance and commercially managed public insurance products such as Medicare Advantage and Medicaid Managed Organizations/Accountable Care Partnership Plans.
Middlemen Pushing Up Retail Costs of Drugs
The reality is that non-price factors, including several players, are causing net prices to decline and retail prices to increase. Those players include employers, health plans, and pharmacy benefit managers (PBMs), all of whom have continuously circumvented the system through loopholes and complicated systems of reimbursement that tend to hurt patients

Telehealth Progress Slowed in 2023
A new report by Cicero Institute, Pioneer Institute, and Reason Foundation reveals worrying stagnation in state-level telehealth expansion efforts in 2023, with only a few exceptions. Progress made during the pandemic is being lost even as provider shortages worsen, raising concerns about patients’ access to care.

Study: High List Prices and Deep Discounts for Prescription Drugs Hurt Poor and Sick Patients
A new Pioneer Institute study illustrates how the current system of drug pricing and discounts leads to patients with challenging diseases being charged huge out-of-pocket sums to keep other premiums low, effectively imposing financial penalties on the sick to protect the healthy and wealthy.

Massachusetts’ Misguided Middle-Class Health Insurance Subsidy Expansion
A proposal on Beacon Hill to expand insurance subsidies up to 500 percent of the federal poverty level, could push the small business insurance market into a death spiral, without reducing the number of uninsured and hurting those with preexisting conditions.
Massachusetts Hospitals: Uneven Compliance with New Federal Price Transparency Law
A 2019 federal law requires hospitals to make prices for 300 shoppable services available online in a “consumer-friendly format,” but a Pioneer Institute survey of 19 hospitals finds that information on discounted cash prices—the price most likely to be charged to consumers paying out of pocket—was unavailable at seven of those hospitals.

Comments on How Pharmacy Benefit Managers (PBMs) affect Smaller Pharmacies and Consumers (ID FTC-2022-0015-0001)
Pioneer Institute Senior Fellows William Smith and Robert Popovian submitted public comments about PBM business practices to the Federal Trade Commission (FTC). Pioneer recommended that PBM discounts be passed along to patients when they are meeting their deductible or coinsurance requirements.
340B Drug Discounts: An Increasingly Dysfunctional Program
This report reviews the federal 340B drug discount program, showing that, over the past decade, the revenue for hospitals generated by the program, initially intended to serve low-income, uninsured populations, has exploded even while a number of important Massachusetts hospitals have reduced the level of charity care they provide. The study notes that nationwide, 340B drug sales rose from $9 billion in 2014 to $38 billion in 2020.
Rating the States on Telehealth Best Practices: A Toolkit for a Pro-Patient and Provider Landscape
The toolkit aims to help policymakers take the next step toward a more quality-oriented, affordable, and innovative health system by ensuring that their state laws on telehealth remove deleterious barriers that have historically discriminated against those in certain geographies, such as those living in rural communities or in underserved urban areas. This report explains policy best practices for ensuring that providers and patients can fully realize the benefits of using telehealth services when appropriate and provides a simple-to-read stoplight rating for each state on how closely their policies align with those best practices.

An Act advancing health care research and decision-making centered on patients and people with disabilities
On November 9th, 2021, William Smith, Pioneer Institute Visiting Fellow in Life Sciences, submitted the following testimony to the Massachusetts Legislature in support of House Bill 201, which addresses a number of flaws and infirmities in the Quality Adjusted Life Years (QALYs) methodology that is utilized by a number of foreign nations in evaluating the value of medicines.
An “Impending Tsunami” in Mortality from Traditional Diseases?
This report examines whether, after the COVID-19 pandemic subsides, the U.S. will have another looming public health crisis emerging from patients failing to have had their cardiology needs addressed properly during the lockdowns. Moreover, if we surmise that a follow-on public health crisis will emerge, we can also conclude that certain population segments are going to be more impacted by CVD, as there are documented health disparities in this therapeutic area. Finally, there are policy changes that could be taken to mitigate a possible spike in CVD adverse events; the paper will close by recommending certain policy changes.
Ten Health Policy Changes That Should Outlive COVID-19
A new study published by Pioneer Institute recommends ten healthcare reforms allowed during COVID-19 that should remain in effect permanently, after the state's emergency declaration for COVID-19 ends on June 15. These reforms have enhanced flexibility in the healthcare system, highlighting barriers that make the system more expensive, harder to access and less patient-centered.

A Brighter COVID Dashboard: State Should Cut Confusion And Clarify All Eldercare Cases and Deaths
Over time, the Massachusetts Executive Office of Health and Human…

The QALY and Cancer Treatments: An Ill-Advised Match
This report examines the alarming methodological and contextual shortcomings of the Quality Adjusted Life Years (QALY)-based methodology in evaluating new cancer therapies. It reveals five specific problems with ICER’s evaluation of cancer treatments and demonstrates the urgent need to prohibit the use of the QALY amid trends in rapid cancer innovations and personalized medicine.
Direct Health Care Agreements: A New Option for Patient-Centered Care That Costs Less and Reduces Provider Burnout
Especially in the COVID era, many are looking to alleviate the increased burden on the healthcare system. One solution is direct healthcare (DHC), which can provide more patient-centered care at affordable prices and is an effective model to increase access to care for the uninsured, underinsured and those on public programs like Medicaid. This paper aims to explain the possible benefits of DHCs, often using DPCs as an example, as they have built a successful record around the country and in Massachusetts.

Healthcare Price Transparency in Massachusetts: Results from a survey of Massachusetts consumers regarding healthcare price transparency
In June 2019, Pioneer Institute, with support from Blue Cross Blue Shield of Massachusetts and the Massachusetts Association of Health Plans, contracted with noted pollster David Paleologos, head of DAPA Research at Suffolk University’s Research Bureau, to conduct a valid and reliable survey of Massachusetts consumers with employer sponsored health insurance. The goals of the survey were to determine consumers’ awareness, attitudes, views, usage, and knowledge of healthcare prices. This white paper presents analysis of the results.
Antimicrobial Resistance: Learning from the current global health crisis to prevent another one
0 Comments
/
The world was blindsided by COVID-19, but a new study finds that…

Five Reasons Why Drug Rebates Are Harmful to Patients and to the Healthcare System
Ever-larger rebates are distorting the market for branded drugs and producing outcomes that often benefit neither consumers nor the healthcare system, according to a new study published by Pioneer Institute.
Analysis of Spending on Shoppable Services in Massachusetts
This report reveals that consumers in just one Massachusetts county could have saved nearly $22 million in a single year and $116.6 million adjusted for inflation over four years if they switched from using the most expensive providers for 16 shoppable healthcare services to those whose prices were closer to average.

Open Letter: COVID-19 Study and Recommendations Task Force established pursuant to Massachusetts Bill H.4672
Recently, Governor Baker signed legislation, H. 4672, that would create a Covid-19 task force, appointed by the legislature, to study and make recommendations to the general court that address health disparities among certain populations based on certain characteristics, including age, and which also asks the future task force to recommend other impacted populations for further study. Pioneer has prepared a public letter to that future task force that contains a list of specific recommendations regarding Covid-19 and the state’s nursing homes.

The Negative Impact of COVID-19 Upon the Biopharmaceutical Sector
Contrary to conventional wisdom that says the coronavirus pandemic will generally benefit biopharmaceutical companies, a new Pioneer Institute study finds many companies will emerge from the pandemic commercially weaker, dealing with delays in new product launches and with fewer resources to invest in research and development.

Status of Healthcare Price Transparency across the United States
At a time when the coronavirus pandemic has caused massive shifts in state policies on telehealth and scope of practice in healthcare, a new Pioneer Institute study underscores that most of the 50 states continue to suffer from weak laws regarding price transparency. The study identified states that have laws that require carriers, providers or both to provide personalized cost information to consumers before obtaining healthcare services.

The Massachusetts Crises Of Care Guidelines Need Re-Thinking
This new study contends that the Massachusetts Department of Public Health’s (DPH’s) Crises Standards of Care (CSC) issued earlier this month bear the earmarks of a state bureaucratic effort. The guidelines need to be rethought under a process that includes a thorough vetting by Massachusetts citizens.

Massachusetts Consumer Healthcare Price Transparency Survey
This public opinion survey, conducted by renowned pollster David Paleologos, Director of Suffolk University’s Research Bureau, focused on consumers’ view of healthcare price transparency. The poll showed that consumers want to know the price of care before obtaining it, and identified opportunities to improve consumers’ search for high-value, low-cost healthcare services.

Looming Challenges for ICER in Assessing the Value of Rare Disease Therapies
This report examines why the Institute for Clinical and Economic Review (ICER) and the Quality Adjusted Life Years (QALY) approach to value assessment is particularly ill-suited to assess the cost-effectiveness of orphan and rare disease treatments, which represent a rapidly growing sector of the biopharmaceutical marketplace.

Wildly Varying MRI Prices at Massachusetts Hospitals: Why We Need Access to Healthcare Prices at All Levels
New study finds there is little correlation between a patient’s out-of-pocket cost and either the amount insurers pay or the overall price of a procedure at 14 representative Massachusetts hospitals.

Key Questions for Legislators on the Institute for Clinical and Economic Review (ICER)
As states continue to grapple with prescription drug costs, a new Pioneer Institute study lays out the key ethical, methodological and disease-specific questions policy makers should address before deciding whether to contract with the Institute for Clinical and Economic Review (ICER) to conduct cost effectiveness reviews used to make decisions about the purchase of medicines and other medical innovations.

MassHealth Protecting Medicaid Resources for the Most Vulnerable
This report finds that Massachusetts' enhanced eligibility verification has allowed MassHealth, the Commonwealth’s Medicaid program, to save significant resources that could be redirected to the care of truly needy Medicaid recipients.

Will New England See Lower Prices from Drug Pricing Transparency Legislation?
This report finds that most new drug pricing transparency laws do not lower consumer out-of-pocket costs, and that expensive and onerous compliance rules would likely put upward pressure on prices. The report reviews recent New England legislative attempts to reduce costs by requiring the disclosure of wholesale drug prices and other information about industry pricing practices.
