Why did some nursing homes experience more COVID-19 deaths and infections than others?
The COVID-19 pandemic has caused great loss for Massachusetts and people across the country. It has been especially deadly and problematic in nursing homes, due to the age of their residents, variability in COVID-19 protocols, and underlying health conditions of elderly patients. When the virus first hit Greater Boston, it was soon apparent that older populations were at higher risk both of contracting the disease and experiencing severe symptoms. To remedy this, some nursing homes and care facilities took precautions and stringent measures to contain the virus and prevent its spread to the extent possible.
COVID long-term care facility tracker.
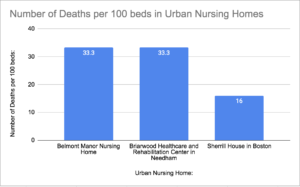
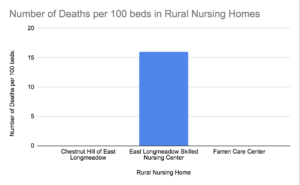
Working with the available data from The Pioneer Institute’s COVID long-term care facility tracker, we can observe trends regarding COVID-19’s impact in nursing homes. As seen in figures 1 and 2, nursing homes in highly populated areas appear to have suffered more deaths and COVID-19 infections than those in less populated, more rural areas, regardless of the number of beds in the nursing home.
https://datausa.io/profile/geo/belmont-ma
https://datausa.io/profile/geo/needham-ma
http://www.city-data.com/city/East-Longmeadow-Massachusetts.html
https://suburbanstats.org/population/massachusetts/how-many-people-live-in-greenfield-town
https://datacommons.org/place/geoId/2507000?utm_medium=explore&mprop=count&popt=Person&hl=en
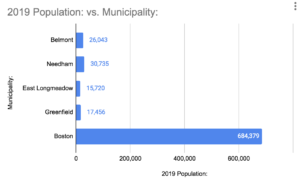
A population map of the communities in which the nursing homes featured in figures 1 and 2 are located can be seen in figure 3. For example, the Sherrill House in Boston (Boston has a population of about 700,000) and the Briarwood Healthcare and Rehabilitation Center in Needham (with a population of about 30,000) have higher mortality rates than nursing homes such as the Chestnut Hill of East Longmeadow and East Longmeadow Skilled Nursing Centers in East Longmeadow (East Longmeadow has a general population of about 15,000).
COVID long-term care facility tracker
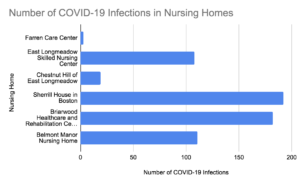
Although there is data showing that population affects COVID-19 infection rates in nursing homes, there was significant variation overall. According to figure 4, many nursing homes, regardless of population and location, experienced high COVID-19 infection and mortality rates.
Another reason for variation in the data is how each specific nursing home followed CDC COVID-19 guidelines. In the Boston area, many nursing homes deployed different measures to help control and remedy high infection rates. According to the CDC, these measures included limiting public visits, limiting contact with other patients, and specific choice of food and cleaning measures. However, some nursing homes did not take CDC guidelines as seriously; caretakers moved between treating infected and non-infected patients, and infected patients were housed with non-infected patients.
Even though trends in COVID-19 infection rates can be observed, the impact of geography on death and infection rates since the start of the pandemic is still not clear. As COVID-19 infection rates decline and more data is collected, it will be important to fully understand the nature and causes of the spread in these facilities to protect nursing home residents from future viruses and avoid the mistakes that took place during the current pandemic.
Nathan Bornstein is a Roger Perry Intern at Pioneer Institute. He is a rising senior high school student at the Buckingham Browne & Nichols school in Cambridge, Massachusetts. His favorite subjects at school are history, math, and foreign language.



