Telemedicine: The Future of Healthcare
Telemedicine sounds a bit like science-fiction, but the practice is far from fictitious. Many Massachusetts doctors practice telemedicine every day, as it is quickly gaining popularity. Telemedicine involves providing healthcare services through technology, rather than in-person (think of a video call, like Skype). What seems like a logical step toward efficiency in healthcare has become a heated debate on Beacon Hill over how to pay for it.
It’s hard to argue against the benefits of telemedicine. First is its convenience: with telemedicine there is no traffic, no babysitter needed, no time taken off work and no gas consumed. With much of the stress of in-person visits eliminated, patients are more likely to seek care. It’s like a return to the house call, only through virtual means.
Beyond convenience, there are several health benefits to telemedicine. The most significant is that the practice increases access to health services, especially primary care and follow-up appointments. Whether for people with hectic schedules, limited time-off from the job, or those unable to drive, telemedicine is the remedy to communicate with doctors from anywhere with an internet connection. For doctors, communication with patients is clear and documented, leading to better patient monitoring and fewer appointment cancellations.
It’s effective to boot. The American Telemedicine Association (ATA) reports that telemedicine is associated with consistent reports of quality service and patient satisfaction. Of course, not all conditions can be diagnosed via telemedicine. In-person visits will still play a vital role in overall healthcare for the foreseeable future, particularly for diagnostic testing. But practicing telemedicine can raise the red flag that brings a patient into the office.
Telemedicine can also reduce the need for certain specialist visits and is usually more efficient than in-person appointments. For example, Blue Cross Blue Shield of Massachusetts reports that a typical telehealth checkup can take only 10 minutes. At Cambridge Health Alliance, their “teledermatology” program allows primary care doctors to send photos of rashes and other skin conditions that patients have to a dermatologist, who replies within 24-hours, thereby eliminating the need for a patient to see a specialist if the photo is sufficient in identifying the condition.
Issue in the Statehouse
While insurers and hospitals alike may support telemedicine, payment for services has become a contentious issue. Hospitals trying to get reimbursement for these services at the same price as in-person visits have faced pushback from insurers, who claim that the cost of delivering telemedicine is lower and should be compensated accordingly. The debate has made its way to Beacon Hill in the form of House Bill No. 267, which would require insurers to reimburse doctors for all telemedicine services, including audio-only and email, at the same rate as in-person visits, as well as specifically include this coverage in all Medicaid and state employee health plans. The bill is supported by the Massachusetts Hospital Association (MHA), which claims it will benefit consumers by saving them the time and stress of physically going to the doctor’s office. The American Telemedicine Association (ATA) agrees, claiming that rather than being represented in lower reimbursement payments, the cost efficiencies of telemedicine will manifest in the more effective management of diseases, preventive care, reduced travel, and fewer or shorter hospital stays.
But the Massachusetts Association of Health Plans (MAHP) says the bill goes too far and would allow doctors to bill for as little as a phone call with a patient, which will significantly cut into any cost savings associated with telemedicine. Even Blue Cross Blue Shield of Massachusetts, which already reimburses video consultations between patients and their doctor or a doctor within network, opposes Bill No. 267, claiming the reimbursement rates shouldn’t be as high as in-person rates.
How it’s done elsewhere
The ATA reported on the status of telemedicine coverage and reimbursement in all 50 states, and gave Massachusetts a “B” grade. While recognizing the absence of a telemedicine “parity law,” or a law guaranteeing the reimbursement of telemedicine at the same rate as in-person services, Massachusetts got points for offering coverage under select Medicaid managed care plans (but not under fee-for-service).
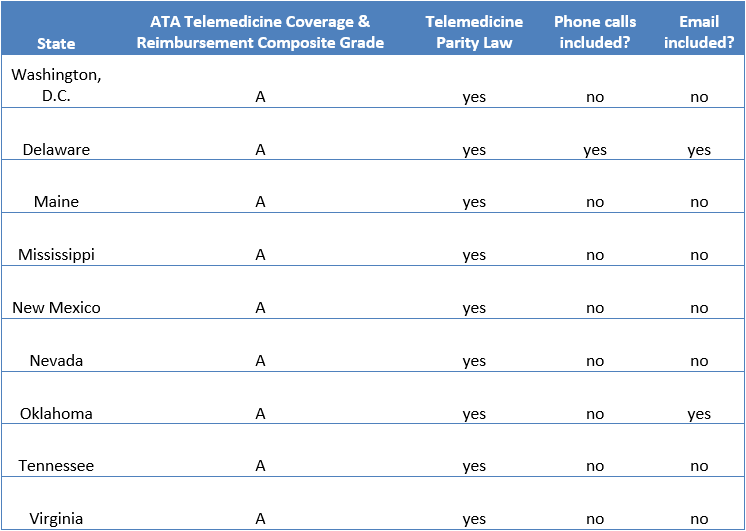
Currently, 28 states and Washington, D.C. have a law requiring the reimbursement of telemedicine at the full, equivalent rate of in-person services. The same ATA report awarded nine of these states a composite “A” for telemedicine coverage. What’s interesting to note is that 8 out of these 9 “A-rated” states do not include telephone calls in their definition of telemedicine, and 7 do not include email either, meaning these states do not require the reimbursement of these services. Oklahoma’s definition includes email, but only Delaware included phone calls and email in their definition, and consequently in their required coverage of telemedicine. Therefore, the reimbursement of telemedicine in most of these states applies only to real-time, audio-visual visits, i.e. video chat. This reimbursement policy likely reflects the offerings (and lobbying) of the large vendors in the telemedicine field.
Looking forward
The question facing Massachusetts is not whether to reimburse telemedicine, but at what rate? Since doctors are performing a service, their time, at the very least, needs to be compensated. The debate will come down to the value of telemedicine: Is a video chat with a doctor the equivalent of an in-person visit? A possible compromise would be to follow the lead of other states and change the definition of “telemedicine” to include interactive audio-visual technology, but not e-mail or traditional phone calls. Another option is to create tier payment levels, one for an in-person visit, one for joint video and audio calls, and one for e-mail or phone calls.
Sadly, this policy debate only serves to highlight how consumer unfriendly our health care system is, as your service and coverage comes down to reimbursement levels and not what is best for the patient.
Wait times are long in Massachusetts, especially in certain parts of the state. We want options that are patient-centered, and increase value. As research gets better on the outcomes of telemedicine, reimbursement rates should be revisited; it may prove to be a better value for certain kinds of medicine, but not others. Legislators should consider including a mechanism to revisit reimbursement levels in the future, outside of the political legislative process.
As the U.S. healthcare system moves away from fee-for-service and toward global payments and integrated care through Accountable Care Organizations (ACOs), the use of technology for communication between providers and patients will likely be a vital piece of care management. Time will tell how many of these institutions embrace telehealth as part of their model, which will reflect its value from both a costs savings and coordinated care perspective, as well as from a consumer service standpoint.
The benefits of telemedicine are undeniable: any practice that increases access and affordability of healthcare should be encouraged. With the Center for Health Information and Analysis (CHIA) set to conduct a cost analysis that will come out this summer, we will soon gain more insight into the financial tradeoffs of reimbursing all forms of telemedicine.
Lauren Corvese recently earned a bachelor’s degree in political science from Northeastern University. In 2015, she joined Pioneer through Northeastern’s co-op program and has continued as a research assistant. Lauren tweets at @laurencorvese