Study: BID-Plymouth Program Shows Promise in Battling Opioid Abuse
Collaborative ER-based approach improves access to detox treatment, reducing relapses and saving money.
BOSTON – Preliminary results suggest that a new program that gives opioid overdose patients at Beth Israel Deaconess Hospital-Plymouth (BID-Plymouth) multiple opportunities to access detox programs, psychological counseling, anti-abuse drugs and other services is proving effective at reducing recidivism and returning opioid users to more productive lives, according to a new policy brief published by Pioneer Institute.
“The Integrated Health Care and Substance Use Collaborative brings together medical personnel, substance abuse specialists and law enforcement to combat this urgent problem in an innovative way that offers a strong model for other hospitals to follow,” said Pioneer Institute Executive Director Jim Stergios.
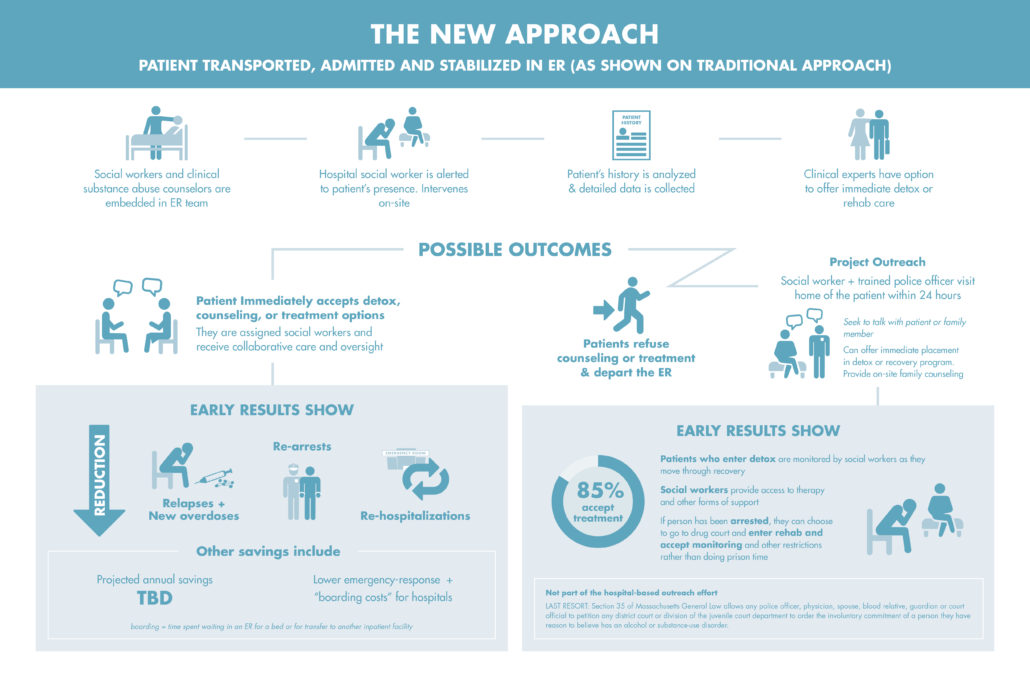
In Combating Opioid Addiction in Massachusetts: A Hospital-Based Solution Shows Promise in Reducing Relapses and ER Costs, author Tom Mashberg describes the process by which a behavioral health team of nurse practitioners, social workers and substance abuse specialists embedded in the emergency room (ER) responds as soon as a patient suffering from an opioid overdose enters the hospital.
The team’s goal is to intervene with the patients at their most vulnerable time, counsel them, and immediately place them in a residential or out-patient treatment program. The team has commitments from community-based detox centers, ensuring that patients will not have to wait days or even weeks for long-term care. Studies show that patients who are forced to wait for access to detox programs are far more likely to continue using opioids than those who are placed rapidly in treatment.
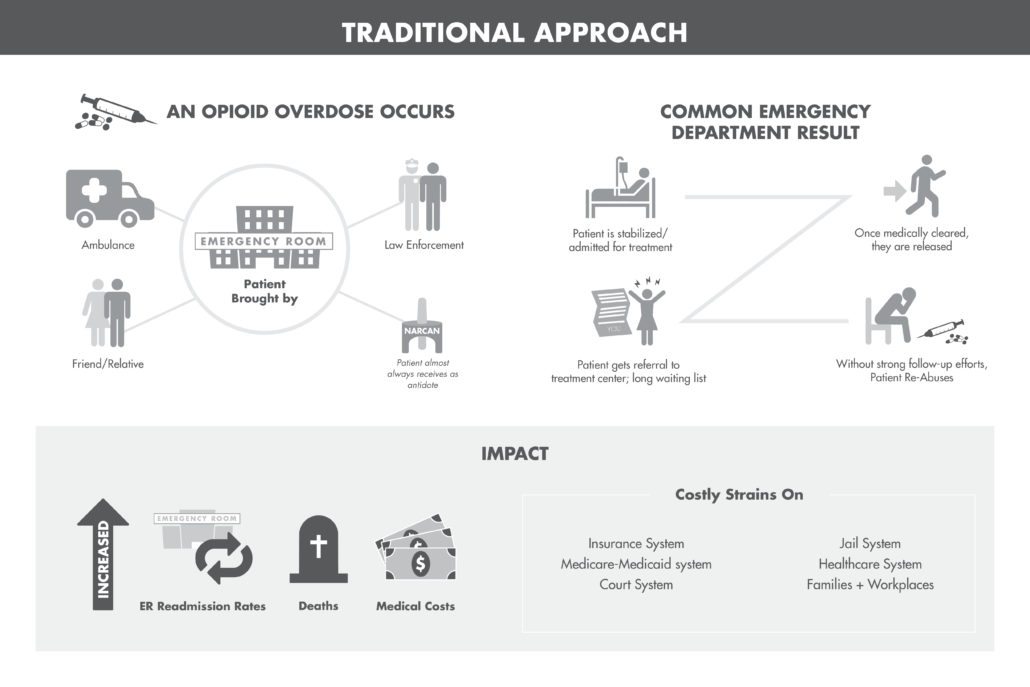
State data show that of the 57,000 Massachusetts emergency department visits attributed to opioid poisonings in 2014, 22,000 were repeat visits, at an average cost of $3,000 to $4,000 per case. Curbing repeat visits offers a substantial savings for hospitals and for MassHealth, which covers 75 percent of the costs of opioid-related ER visits.
An added and innovative component contributes to the success of the BID-Plymouth program. If the overdose patient refuses counseling on-site and departs the ER, substance abuse counselors and local police arrange to visit him or her within 12-to-48 hours, armed with a commitment from local detox centers that the patient can be driven directly to the site for admission. Early data show that 85 percent of patients visited post-discharge have agreed to enter treatment.
Experts and state officials estimate conservatively that opioid abuse costs Massachusetts taxpayers upwards of $1.5 billion annually, when healthcare, criminal justice and other costs are taken into account. In addition to getting opioid abusers into treatment, the collaborative can save money because the cost of adding substance abuse specialists to hospital staffs pales in comparison to the savings from reducing recidivism and other preventive measures.
For example, many opioid patients require 24 to 72 hours of hospital boarding time to receive treatment and recover from their overdose, which can cost up to $10,000. BID-Plymouth is in the initial stage of data collection and hopes to have fuller information within two years. A portion of a $3.7 million state mental health grant helped pay for the hiring and training of hospital personnel.
 In Combating Opioid Addiction in Massachusetts, Mashberg recommends that hospitals across the state carefully track the amount of opioids they dispense and aggressively limit prescriptions. Hospitals also must accelerate their real-time monitoring of opioid prescriptions by investing in a coordinated database that can reduce the incidence of multiple prescriptions falling into the hands of users or dealers who circulate among hospitals.
In Combating Opioid Addiction in Massachusetts, Mashberg recommends that hospitals across the state carefully track the amount of opioids they dispense and aggressively limit prescriptions. Hospitals also must accelerate their real-time monitoring of opioid prescriptions by investing in a coordinated database that can reduce the incidence of multiple prescriptions falling into the hands of users or dealers who circulate among hospitals.
Other recommendations include state support for hospital-based efforts to staff ERs with addiction specialists and others who can intervene and offer opioid users access to treatment, and following through on a state commitment to add several hundred new detox beds over the next two years.
State legislation passed in March devotes more than $250 million to combat the opioid crisis with treatment, education, prevention and recovery, and bulk purchases of drugs used as overdose antidotes and for drug detoxification.
In 2000, there were 338 opioid-related deaths in Massachusetts, or 5.3 per 100,000 people. By 2015 that number had more than quadrupled to 1,536 deaths, or 22.6 per 100,000 people.
The policy brief is based on an entry that is a runner-up in Pioneer Institute’s 2016 Better Government Competition, the theme of which is “Improving the quality and access to care for individuals living with mental illness.”
Tom Mashberg is a veteran investigative reporter and editor specializing in coverage of the opioid crisis. He was a 2014 Pulitzer Prize co-finalist for The Record of North Jersey for reporting on opioid and heroin addiction in New Jersey. With fellowship funding from the McGraw Center for Business Journalism at the City University of New York’s Graduate School of Journalism, Mashberg is examining the pharmaceutical industry’s role in the opioid industry.
About Pioneer: Pioneer Institute is an independent, non-partisan, privately funded research organization that seeks to improve the quality of life in Massachusetts through civic discourse and intellectually rigorous, data-driven public policy solutions based on free market principles, individual liberty and responsibility, and the ideal of effective, limited and accountable government.