Massachusetts Should Disclose More Information about Its Recent Reduction in the Official Count of Long-term Care Deaths
Pioneer Institute takes note of the state’s recent substantial reduction in total long-term care deaths, which the state attributes to adoption of a narrower federal standard for long-term care reporting. Prior to adopting this new standard, the state reported, on April 14, a total of 9,018 deaths in long term care facilities as posted on its Daily Dashboard. An April 23 Boston Globe article reported that after applying this narrower federal standard, the state reported, on April 15, that nursing home deaths totalled 5,502, a drop of more than 3,000 deaths.
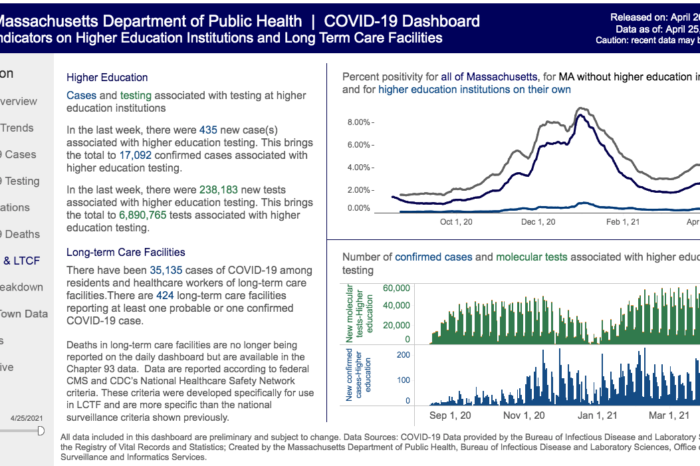
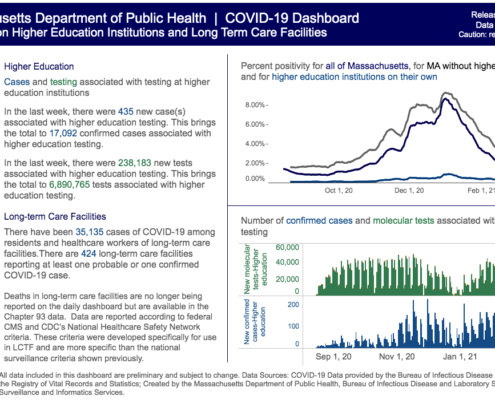
According to the state’s COVID-19 Dashboard, this narrower federal standard is the CDC’s “National Healthcare Network Safety Criteria“, which the state describes (in something called the Chapter 93 Elder Facility Aggregative Report) as capturing “confirmed COVID-19 diagnoses and COVID-19 related deaths as reported by Massachusetts elder facilities.” The standard itself says (on page 11) that its goal is to capture deaths “from SARS-COV-2 (COVID-19) related complications.”
At the same time, the state has maintained an apparently-broader standard for the Dashboard’s count of overall COVID-19 deaths in the state’s population. The state has described this to Pioneer, and the Boston Globe, as a CDC-authorized “surveillance” standard. As to its substance, the April 23 Globe article states (consistent with what the state had earlier told Pioneer as well), that DPH previously used a “sweeping definition for COVID deaths in long-term care. It was counting any resident or staff who contracted COVID at any time prior to their death in a nursing home or a hospital or rest home. Even those who tested positive but later died of an apparently unrelated cause were counted as a nursing home COVID death.” We do not know if that the same broad standard was used for counting all COVID-19 deaths, and we cannot independently identify the standard that has been used for that count during this pandemic. Regardless, the state’s approach to counting overall COVID-19 deaths must be far more expansive than the National Healthcare Network Safety Criteria standard, because the former appears to count thousands of deaths that are excluded by the latter.
The issues in this area appear to be evolving, with the Boston Globe running two stories on the topic in the last week. Nonetheless these issues are clearly important, because clarity about COVID-19’s impact in eldercare communities is crucial.
Indeed, Pioneer itself has played a role in the present developments: starting in December 2020, it has been asking the state questions about its count of eldercare deaths, and those questions may well have prompted the recent changes.
In any event, Pioneer Institute believes that the state should promptly provide information in the following areas, to allow a meaningful assessment by the public, and, as necessary, by relevant subject-matter experts:
-
- As to the special standard for counting long-term care deaths (the National Healthcare Network Safety Criteria), that standard itself seems sensible. However, the state should provide information about its adoption and implementation of that standard, to ensure that eldercare deaths are not being undercounted. The state says that under this standard it has “removed” thousands of deaths where the resident had previously “recovered” from COVID-19. (See page 3 of this April 22 Weekly Public Health Report.) But this is not a black and white issue: the National Healthcare Network Safety standard itself (at page 11) says that it is meant to encompass deaths from “complications” of COVID-19. Is the state ensuring that such deaths – i.e., ones that followed complications from a “previous” COVID-19 infection — are included in the tally of eldercare deaths? We are hopeful that the answer is yes, but the question is fair given the sudden and substantial change in numbers at issue. The state should disclose the guidance it has provided to relevant personnel on this point.
- As noted, the state has apparently maintained a broader, “surveillance” standard for counting overall deaths in the state. While the state’s COVID-19 Dashboard specifically identifies the standard for long-term care, and provides a link to it (see the “Higher Ed and LTCF [Long-term Care Facilities” section of the Dashboard), the Dashboard does not do the same for the surveillance standard it uses for counting overall deaths. The Dashboard describes a methodology, but does not state or link to any formal standard from which that methodology derives. It should do so in the section shown here:
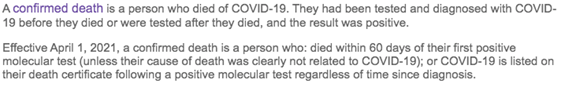
- Relatedly, as shown in the image above, the Dashboard states that the described methodology for counting overall deaths is “Effective April 1, 2021.” Was a different methodology in use before April 1? If so, the state should obviously identify that too. It is unacceptable that the public does not know, clearly, how the state has been counting COVID-19 deaths during this pandemic.
- The state should also explain what specifically there is about the varying standards that leads to such different numerical results in deaths in long term care facilities. The state’s application of the narrower, long-term care standard has resulted in the removal of thousands of deaths from the former tally of long-term care deaths. Those same deaths appear to remain in the tally of overall deaths in the state. It appears, then, that the two standards lead to very different results, with the former excluding thousands of deaths that the latter encompasses. What is the precise mechanical difference between the standards that has so profound an impact? What are representative examples of deaths that are excluded by the long-term care definition, but encompassed within the overall-deaths definition? The state must know, and should disclose this precise practical difference. This would enhance public confidence, and allow assessment — by experts as necessary — of whether the state is counting correctly. In addition, there is yet another wrinkle in the state’s recounting of nursing home deaths which has not been fully explained or officially reported. According to a Globe article published on April 24, the state asked nursing home administrators to take another look at the cause of deaths and to reclassify COVID-19 deaths if warranted, using the narrower definition. One problem with this directive is that the threshold language in the narrow standard now identified on the Dashboard (the National Healthcare Network Safety Criteria) is almost the same language as the definition used in the state’s Aggregative Report, language that nursing home administrators were presumably to use in reporting deaths in the first place. So it’s not at all clear to the public what administrators were to do differently. However, whatever they did, it resulted in further lowering the death numbers in long term care facilities, as reported in the April 24 Globe article, to 5,502. Clearly, much more explaining and transparency needs to be shed on this process before such a result can be accepted by the public.
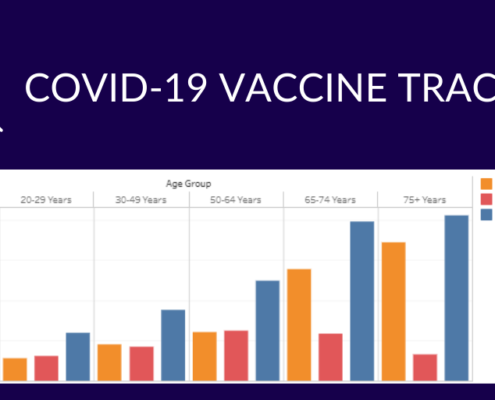
- Finally, the state should address a significant problem. If indeed the total number of long-term care deaths is being tallied under a restrictive standard, and the total number of overall deaths is being tallied under an expansive standard, that could create a significant public misimpression on an important metric: the proportion of eldercare deaths to all deaths. Before, the Dashboard reported long-term care deaths in excess of 9,000 — or more than 50 percent of all deaths in the state. Now, using the Boston Globe’s reported number of nursing home deaths (5,502), the equivalent percentage is approximately 32 percent.
But that latter, much smaller percentage appears to be driven by a classic apples to oranges problem: as explained here, and covered by the Globe’s recent articles, the state appears to be using a special, restrictive standard for counting long-term care deaths, while maintaining a more expansive standard for counting overall deaths. Thousands of eldercare deaths are being removed from the numerator, and left in the denominator. Is this indeed what is happening?
Importantly, it is not enough for the state to simply identify federal standards aligning with the current approach to counting long-term care deaths, and overall deaths, respectively. Even if both approaches are well-grounded in federal standards (which we don’t yet know), an apples-to-oranges problem remains. In that case, Massachusetts should at minimum state on the Dashboard that the eldercare tally cannot be compared to the tally of overall deaths. It should also explain this apples to oranges problem to the federal government, and work with appropriate officials toward a solution. There must be a way for eldercare COVID-19 deaths to be reported in a manner that properly aligns with overall COVID-19 deaths, and allows the public to see how the former compares to the latter.
****
Counting COVID-19 deaths is surely a complex matter, and Pioneer Institute acknowledges that different approaches may exist, and that they may serve different legitimate purposes. However, the public — particularly in Massachusetts, where COVID-19’s toll on elders has been so great — has a right to know how many deaths occurred in state-regulated eldercare facilities, and how that compares to the total number of deaths. However well-intended, a counting regime that clouds this fundamental fact is flawed, and should be corrected — or at minimum clearly disclosed to the public.
Get Our COVID-19 News, Tips & Resources!
Related Posts: